NHADACA Announcements

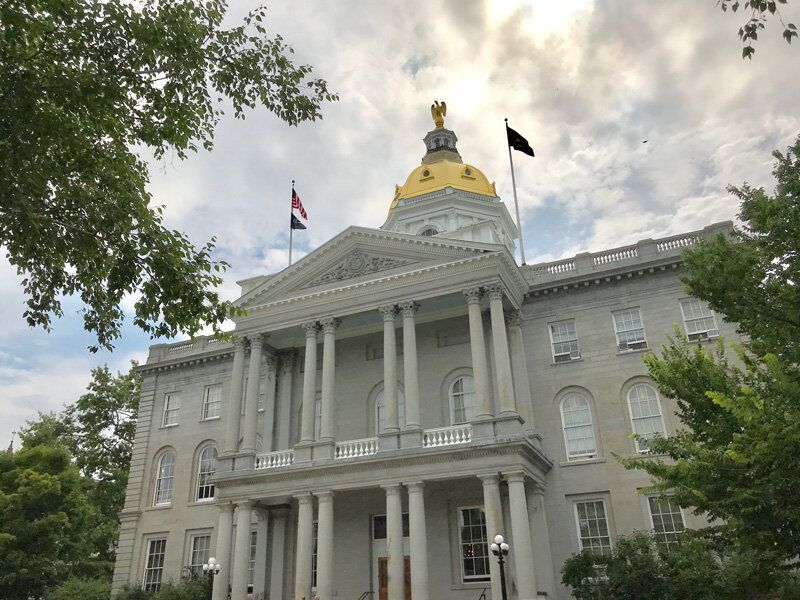
Governor Kelly Ayotte has signed House Bill 507 into law, a major step forward in improving access to mental health care across the state. Starting January 1, 2026, health insurers will be required to process credentialing applications from mental health professionals within 30 days—matching the timeline already in place for primary care providers. This legislation, championed by the New Hampshire Insurance Department (NHID) and supported by healthcare leaders and mental health advocates, removes a key administrative barrier that has delayed care for many Granite Staters. “This law brings mental health help closer to home for more people, faster,” said Insurance Commissioner DJ Bettencourt. “It strengthens our workforce and ensures qualified providers can get to work without unnecessary delays.” The NHID will continue working with insurers and providers to ensure a smooth rollout of the new requirements. Learn more at insurance.nh.gov .
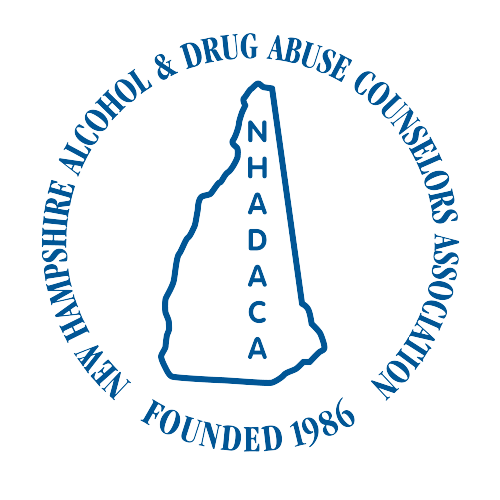
The Governor’s Commission on Alcohol and Other Drugs is seeking to gather information from professionals, those with lived experience around substance use, and all New Hampshire residents to inform strategic decisions around Alcohol Fund investments. There will be four opportunities for participation: Attend the in-person public forum on Tuesday, April 15th at NHTI – Sweeney Auditorium 122 (31 College Drive, Concord, NH 03301) from 4:00-6:00 pm. Attend the in-person public forum on Wednesday, April 16th at The Rocks – Jane Difley Classroom (113 Glessner Rd, Bethlehem, NH 03574) from 4:00-6:00 pm. Attend the online public forum on April 22nd via Z oom from 4:00-6:00 pm. Provide your thoughts on your own time via this sho rt survey . For more information, visit https://nhcenterforexcellence.org/governors-commission/ .

ADMINISTRATIVE COORDINATOR Description Fulltime position for Administrative Coordinator at a membership association for addiction professionals. The Administrative Coordinator works with immediate supervisor, the Executive Director, and the various program leads in supporting each of NHADACA’s programs through a wide range of administrative duties and tasks. The ideal candidate would be organized, detail-oriented, and capable of multitasking while maintaining excellent communication with both internal and external stakeholders. Requirements High school diploma with at least 3 years administrative support experience Solid time-management abilities with the ability to prioritize tasks Adaptable with ability to work independently as well as in collaborative roles Ability to focus in an open work area with frequent interruptions Strong problem-solving, planning, organization and communication skills Basic math abilities with an understanding of basic financial concepts Computer skills sufficient to use programs such as MS Office applications, survey platforms, meeting platforms, Constant Contact, QuickBooks, payment applications, and nonprofit website and customer relations platforms such as Neon One Ability to meet light to medium physical demands of occasional training support to include moving chairs and tables, light cleaning and trash removal Professional appearance and courteous manner Duties Support the general functions of the NH Alcohol & Drug Abuse Counselors Association and its varied programs: the NH Training Institute on Addictive Disorders (NHTIAD), the Clinician Wellbeing Network (CWN), and the Credentialing Support Partnership (CSP) such as addressing client queries (via email, phone and in-person), managing and routing phone calls and distributing incoming mail Conduct monthly revenue reconciliation reports, QuickBooks accounting processes, invoices and similar accounts payable and receivable functions Scheduling meetings, conference and training room reservations and maintaining related calendars Monitor and track office equipment and equipment purchases, ensuring it is properly maintained or serviced when needed Organize and maintain filing systems (digital and physical) ensuring the proper archiving of company records Training participant support including tracking attendance, payment/refunds, registration, sign/check in for in-person trainings, and data management within the Neon One CRM Attend training team meetings to facilitate communication and collaboration on above training activities Webinar, lunch & learn and peer collaboration scheduling, participation tracking and support for the Credentialing Support Partnership and Clinician Wellbeing Network Manage survey processes including creation and data aggregation for NHADACA projects such as annual surveys, membership and board surveys, and surveys related to webinars, lunch and learns and peer collaboration Support registration processes for the annual NH Behavioral Health Summit Other duties as assigned by immediate supervisor and the Executive Director How to Apply Send email with resume to Dianne Castrucci, Executive Director ( dianne@nhadaca.org )

NHADACA's Clinician Wellbeing Network offers monthly groups, topics include: Grief and Loss - 2nd Wednesday from 8:00am-9:00am; virtual; for clinicians experiencing grief and loss. Wellness - 1st Wednesday from 8:00am-9:00am; virtual; for all clinicians. Open Discussion - 3rd Thursday from 9:30am-11:30am; virtual; for all clinicians. Independent Practice - 3rd Wednesday from 8:00am -9:00am; virtual; for those in or intending to be in a private practice. Clinical Supervisors - 4th Thursday 12:00pm-1:00pm; virtual; for MLADCs providing clinical supervision Vicarious Trauma - TBA

We’re thrilled to welcome two exceptional new members to our Board of Directors! Please join us in welcoming Robert Meshna and Ivysue Hranac. Their expertise and commitment to our mission will be invaluable as we continue to expand our impact and strengthen our community. Robert Meshna, LADC, CRSW, NCPRSS - The Doorway of Greater Nashua. Biography: I have worked in the substance use/behavioral health field for 13 years. I started my career in Florida working in inpatient substance use treatment facilities. I moved to New Hampshire where I met my wife and now have a two-year-old son. I continued to work in a local inpatient treatment facility and eventually found my way to the Doorway of Greater Nashua in 2020. I obtained my NCPRSS with NAADAC in 2018. I have been a licensed CRSW since 2019 and became a CRSW supervisor in 2022. I recently obtained my LADC in May 2024. I graduated from SNHU summa cum laude with a bachelor’s in human services with a concentration in substance use. I am currently enrolled in a Master of Social Work program at UNH. I have worked at the Doorway of Greater Nashua for over 4 years helping people access treatment and providing recovery support services. I enjoy advocacy work, helping people into and maintain recovery, and helping with professional and personal growth. I enjoy spending time with family, traveling, doing yard work and DIY projects. Statement of interest: I would love the opportunity to join the board to help other students through any questions about licensing career guidance, professional development. Sharing personal experiences and experiences of others can normalize and positively reinforce people’s goals and aspirations during what can be anxiety provoking times. I experienced limited career guidance with many schools when deciding which school to attend and there were many limitations that advisors faced when guiding students. Many of these experiences have also been shared by my peers and colleagues over the years. I also experienced challenges in the licensing process and wish I had someone to help me through them. Ivysue Hranac, LICSW - Rockingham County Department of Corrections Biography: Ivysue currently works at Rockingham County Department of Corrections as the Mental Health Supervisor. She has worked with individuals who have mental health issues as well as cooccurring issues. She has been a case manager, intern, clinician and supervisor/program director prior to her current role. In her former role she was the program director for a program which placed individuals who were incarcerated for dangerous crimes and had a mental health issue into the community for re-integration. Currently she is working on obtaining her MLADC credentials. She has a Bachelor's degree in Criminal Justice and a MSW from the University of Wyoming and is a Licensed Independent Clinical Social Worker in New Hampshire and Washington state. She has worked in the mental health field for 14 years and believes in bringing a humanistic approach to her work. She has provided training in Motivational Interviewing and continues to use this experience as she works with individuals who are incarcerated. She is raising two of her grandchildren with her partner and recently moved back to New Hampshire from Washington. Statement of interest: I would like to serve on the NHADACA board because I am excited to be in community with other individuals who believe in the mission of NHADACA. I look forward to discussions with people who have more knowledge than I do about the SUD system and how we can support all SUD clinicians to better the outcomes of the humans we work with. I have personal as well as professional insight into some of these issues and would hope to be helpful in shaping our state to be a leader in the SUD and Co-occurring milieu.
The Contract Lifecycle is a series of finance trainings designed for those who contract with the NH Department of Health and Human Services (DHHS). Register for upcoming sessions below! There is no fee to register or attend any of these finance training sessions as this finance training series has been made available through funding by the Bureau of Drug & Alcohol Services in collaboration with the NH Charitable Foundation.
On August 8, 2024, the LADC Board adapted the revised Alc 400 rules, which will take effect in 60 days. The public has 30 days to email the LADC Board with any questions or concerns pertaining to the new rules. Additionally, The LADC Board also advised that they are re-opening the Alc 300s again. Follow the process below, per the Office of Professional Licensure and Certification (OPLC), to submit a request: Plc 209.01 Requests for Explanation of Adopted Rules . (a) Any interested person may, within 30 days of the final adoption of a rule, request a written explanation of that rule by making a written request to the executive director, for any rule in title Plc, or to the board that adopted the rule, for rules in any title other than Plc. (b) A request submitted pursuant to (a), above, shall include: (1) The name and address of the person making the request and, if the requestor is an entity, the name, address, and email address of the individual authorized by the entity to make the request; and (2) Identification of the specific rule for which an explanation is sought. Click here to review the revised changes.

Join more than 1,500 addiction professionals in Washington, DC for the NAADAC 2024 Annual Conference & Hill Day from October 18 to 23, 2024! Engage in learning, networking, advocacy, and success. NAADAC's 2024 Conference offers a comprehensive six-day educational event focused on addiction, featuring intensive training sessions by renowned experts, a day dedicated to advocacy on Capitol Hill, poster presentations, an expansive exhibit hall, special events, ample networking opportunities, and many additional activities! The NHADACA Board of Directors awards 2 of our members with a scholarship to attend this event annually. As a NHADACA member, you can submit a scholarship application by July 22, 2024. Scholarship Application You can read more about this event here: https://www.naadac.org/annualconference
The University of Rhode Island offers access to six free continuing education modules for healthcare professionals on substance use disorders (SUD), requesting bulk naloxone for distribution to your community, and/or requesting a free "live" overdose response training seminar for your group or organization. Seminars are offered via Zoom and are geared towards the general public or can be accredited for 1 hour of live CEU for healthcare professionals (live CEU available for pharmacists, nurses, social workers, or licensed mental health counselors). Learn more here: https://web.uri.edu/rota-r/

A new report, released by SAMHSA, explores the financing, utilization, and regulatory structures of providing peer recovery support services (PRSS) for substance use disorder (SUD) recovery process within federal grant programs and state Medicaid programs. This report identifies challenges and opportunities to finance and strengthen the PRSS workforce. It also provides a description of the variation in peer recovery rates, supervision, credentialing, and substance use disorder vs mental health. You can find it here: https://www.samhsa.gov/cfriutm_source=SAMHSA&utm_campaign=935ab5c617EMAIL_CAMPAIGN_2024_04_08_05_20&utm_medium=email&utm_term=0_-935ab5c617-[LIST_EMAIL_ID] In addition, SAMHSA also released a webinar covering the same topic. You can access the webinar here: https://www.youtube.com/watch?v=jyMr6SA5Hy4

New Opportunity for Master Licensed Alcohol and Drug Counselors (MLADCs) and expansion of care! Effective January 1, 2024: Treatment and Billing by Mental Health Counselors (MHC) has been approved through the Centers for Medicare and Medicaid Services (CMS) With the publication of the new rules for CMS billing and services reimbursement, mental health counselors (MHC) can officially enroll in Medicare and begin to treat individuals with substance use disorders and mental health conditions. The term “mental health counselor” is defined broadly to include licensed and certified professional counselors, as well as addiction counselors and alcohol and drug counselors. Eligibility requirements specify that individuals: (1) have a master’s or doctorate degree in counseling, (2) are licensed or certified by the state in which they furnish services, and (3) have performed at least 2 years or 3000 hours of supervised clinical experience after obtaining their degree. For an brief overview of the updates for eligibility requirements for addiction professionals, please review https://www.cms.gov/medicare/payment/fee-schedules/physician-fee-schedule/marriage-and-family-therapists-mental-health-counselors . A more comprehensive update for the rules can be found at https://www.govinfo.gov/content/pkg/FR-2023-11-22/pdf/2023-24293.pdf . While there are some limitations with billing for Medicare services based on level of care (specifically for IOP/PHP programs), this is a positive step towards recognizing and supporting the treatment of substance use disorders (SUD) in the State of New Hampshire. The approved billing services include: Bundled substance use disorder (SUD) payments for: SUD management and counseling SUD services provided in an office setting, including: Overall management Care coordination Individual and group psychotherapy Substance use counseling